Learn more about common chronic pain conditions and how our expert pharmacists can help you to better manage your symptoms.
Pain Management Resources & Expert Help | Walgreens


Live life with
less pain
Learn more about common chronic pain conditions and how our expert pharmacists can help you to better manage your symptoms.
Our pharmacists
are specially trained in pain management
- Meet one-on-one for free pain management consultations
- Get personalized recommendations for treatment
- Learn about our wide range of pain management solutions


Our pharmacists
are specially trained in pain management
- Meet one-on-one for free pain management consultations
- Get personalized recommendations for treatment
- Learn about our wide range of pain management solutions

Arthritis explained
Learn more about the causes and symptoms of arthritis and ways to treat it.
- What is arthritis?
Arthritis is inflammation of the joints. There are more than 100 different types of arthritis.
- What are risk factors for arthritis?
There is no single cause of arthritis. Many factors can lead to arthritis, including genetics, age, gender, lifestyle and environment.
- What are the two common types of arthritis?
The two main types of arthritis are:
Rheumatoid (RA): A chronic disease that causes joint pain, stiffness, swelling and limited movement of the joints.
Osteoarthritis (OA): A chronic disease of the whole joint in which bones in impacted joints become frailer, the connective tissue that holds the joint together deteriorates and swelling damages or wears away the joint lining.
- How is arthritis diagnosed?
Arthritis is diagnosed in a number of different ways. Your healthcare provider will gather information and can do a physical exam WITH basic tests to check for arthritis.
Your health care provider will gather your medical history and ask questions about your symptoms, general health, family history and habits.
If your symptoms are more complex, you may need to see a rheumatologist (a doctor who specializes in arthritis and autoimmune diseases) or an orthopedist (a doctor who specializes in deformity disorders affecting bones, joints, and muscles).
Other tests used to diagnose arthritis include a joint evaluation, lab tests and imaging tests, such as X-rays.

Live life with
less pain
Learn more about the causes and symptoms of arthritis and ways to treat it.
- What is arthritis?
Arthritis is inflammation of the joints. There are more than 100 different types of arthritis.
- What are risk factors for arthritis?
There is no single cause of arthritis. Many factors can lead to arthritis, including genetics, age, gender, lifestyle and environment.
- What are the two common types of arthritis?
The two main types of arthritis are:
Rheumatoid (RA): A chronic disease that causes joint pain, stiffness, swelling and limited movement of the joints.
Osteoarthritis (OA): A chronic disease of the whole joint in which bones in impacted joints become frailer, the connective tissue that holds the joint together deteriorates and swelling damages or wears away the joint lining.
- How is arthritis diagnosed?
Arthritis is diagnosed in a number of different ways. Your healthcare provider will gather information and can do a physical exam WITH basic tests to check for arthritis.
Your health care provider will gather your medical history and ask questions about your symptoms, general health, family history and habits.
If your symptoms are more complex, you may need to see a rheumatologist (a doctor who specializes in arthritis and autoimmune diseases) or an orthopedist (a doctor who specializes in deformity disorders affecting bones, joints, and muscles).
Other tests used to diagnose arthritis include a joint evaluation, lab tests and imaging tests, such as X-rays.
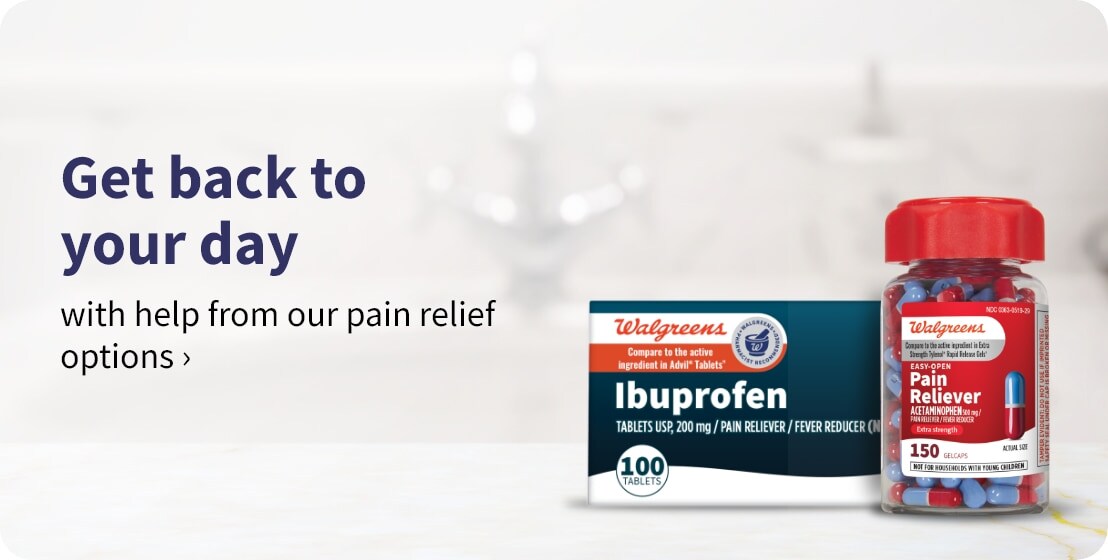
How do you treat arthritis?

Exercise & weight loss

Topical pain relievers

Oral Non-steroidal anti-inflammatory drugs (NSAIDs)

Prescription NSAIDs

Joint Injections

Disease-modifying anti-rheumatic drugs (DMARDs)

Non-steroidal anti-inflammatory drugs (NSAIDs) Corticosteroids

Biologics agents
Expert tip & articles

Managing headaches & migraines
While these conditions may be similar, they have unique causes and treatment options.
- What is a headache?
A headache is a pain in your head or face. That pain can be throbbing, constant, sharp, or dull.
- What are common headache triggers?
Common headache triggers include:
- Stress
- Diet
- Weather changes
- Caffeine withdrawal and abrupt discontinuation of medications that contain caffeine
- Lack of sleep
- Fatigue
- Hunger
- Treatment options for headaches
One of the most important parts of treating headaches is figuring out your triggers. Learning what those are can help reduce the number of headaches you have. Try keeping a log of your headaches when they occur and note what you think caused them.
Once you know your triggers, your healthcare provider can tailor your treatment, whether that's drug-free treatments (acupuncture, meditation, biofeedback, relaxation therapy), over-the-counter pain relievers, or prescription medications.
- What is a migraine?
A migraine is a severe headache with throbbing pain or a pulsating sensation accompanied by additional symptoms such as nausea, vomiting, and sensitivity to light or sound. Migraines may last several hours to days and the pain can hinder daily activities. Headaches must have occurred on at least five occasions and lasted for 4–72 hours (when not treated) each time to be considered a migraine. The headache must also have two of the following symptoms: moderate or severe pain, pain on only one side of the head, a pulsing or throbbing sensation, or pain that’s made worse by movement or physical activity.
- What causes migraines?
Genetic and environment factors may play a role in migraines.
Additionally, certain factors increase your risk of migraines, including being female, having a family history of migraines or having other health conditions including depression, anxiety, bipolar disorder, epilepsy or sleep problems.
Each person has different migraine triggers but the most common ones are listed below. If you can identify your triggers and avoid them, you may be able to more effectively manage your migraine and avoid future migraine attacks.
- Stress
- Changes to your sleep schedule
- Hormones
- Caffeine and/or alcohol
- Diet
- Dehydration
- Light
- Smell
- Overuse of medication
- Treatment options for migraines
While there’s no cure for migraines at this time, treatments can offer you relief. Over-the-counter medications such as acetaminophen (Tylenol), a combination of acetaminophen, aspirin, and caffeine (Excedrin), naproxen (Aleve) and ibuprofen (Advil, Motrin), may help ease mild to moderate migraines.
Your provider may recommend that you take prescription medication daily to reduce your migraines. Several types of medications are used to prevent migraines, such as beta blockers and other cardiovascular medications, antidepressants, and more. Your provider may recommend botulinum (Botox) injections for migraines if you have chronic migraines.
Limited studies show that certain supplements, including butterbur, magnesium, feverfew, coenzyme Q10, and riboflavin may be beneficial in migraine prevention. However, it’s important to note that many of these studies were small and results were inconsistent.
Making changes to your daily routine may also help to keep migraines at bay. Try to:
- Get enough sleep
- Exercise regularly
- Eat regular meals and do not skip meals
- Drink plenty of water
- Take actions to reduce stress
- Avoid migraine triggers

Managing headaches & migraines
While these conditions may be similar, they have unique causes and treatment options..
- What is a headache?
A headache is a pain in your head or face. That pain can be throbbing, constant, sharp, or dull.
- What are common headache triggers?
Common headache triggers include:
- Stress
- Diet
- Weather changes
- Caffeine withdrawal and abrupt discontinuation of medications that contain caffeine
- Lack of sleep
- Fatigue
- Hunger
- Treatment options for headaches
One of the most important parts of treating headaches is figuring out your triggers. Learning what those are can help reduce the number of headaches you have. Try keeping a log of your headaches when they occur and note what you think caused them.
Once you know your triggers, your healthcare provider can tailor your treatment, whether that's drug-free treatments (acupuncture, meditation, biofeedback, relaxation therapy), over-the-counter pain relievers, or prescription medications.
- What is a migraine?
A migraine is a severe headache with throbbing pain or a pulsating sensation accompanied by additional symptoms such as nausea, vomiting, and sensitivity to light or sound. Migraines may last several hours to days and the pain can hinder daily activities. Headaches must have occurred on at least five occasions and lasted for 4–72 hours (when not treated) each time to be considered a migraine. The headache must also have two of the following symptoms: moderate or severe pain, pain on only one side of the head, a pulsing or throbbing sensation, or pain that’s made worse by movement or physical activity.
- What causes migraines?
Genetic and environment factors may play a role in migraines.
Additionally, certain factors increase your risk of migraines, including being female, having a family history of migraines or having other health conditions including depression, anxiety, bipolar disorder, epilepsy or sleep problems.
Each person has different migraine triggers but the most common ones are listed below. If you can identify your triggers and avoid them, you may be able to more effectively manage your migraine and avoid future migraine attacks.
- Stress
- Changes to your sleep schedule
- Hormones
- Caffeine and/or alcohol
- Diet
- Dehydration
- Light
- Smell
- Overuse of medication
- Treatment options for migraines
While there’s no cure for migraines at this time, treatments can offer you relief. Over-the-counter medications such as acetaminophen (Tylenol), a combination of acetaminophen, aspirin, and caffeine (Excedrin), naproxen (Aleve) and ibuprofen (Advil, Motrin), may help ease mild to moderate migraines.
Your provider may recommend that you take prescription medication daily to reduce your migraines. Several types of medications are used to prevent migraines, such as beta blockers and other cardiovascular medications, antidepressants, and more. Your provider may recommend botulinum (Botox) injections for migraines if you have chronic migraines.
Limited studies show that certain supplements, including butterbur, magnesium, feverfew, coenzyme Q10, and riboflavin may be beneficial in migraine prevention. However, it’s important to note that many of these studies were small and results were inconsistent.
Making changes to your daily routine may also help to keep migraines at bay. Try to:
- Get enough sleep
- Exercise regularly
- Eat regular meals and do not skip meals
- Drink plenty of water
- Take actions to reduce stress
- Avoid migraine triggers
Making changes to your daily routine may also help to keep migraines & headaches at bay. Try to:

Get enough sleep

Exercise regularly

Eat a healthy diet

Drink plenty of water

Reduce stress

Limit caffeine
Expert tip & articles

Understanding chronic pain
Chronic pain can come in many forms. Learn more about common causes and treatment options.
- What is chronic pain?
Chronic pain is usually defined as any pain that lasts longer than three months This pain may occur all of the time or may come and go periodically. Chronic pain may affect people to the point that they cannot work, eat properly, take part in physical activity, or fully enjoy life.
- What is the difference between chronic pain and acute pain?
Acute pain happens when you get hurt, such as a cut or a broken bone. It doesn’t last long, and it goes away after your body heals from whatever caused the pain. Chronic pain, however, continues long after you recover from an injury or illness.
- What causes chronic pain?
One of the most important parts of treating headaches is figuring out your triggers. Learning what those are can help reduce the number of headaches you have. Try keeping a log of your headaches when they occur and note what you think caused them.
Once you know your triggers, your healthcare provider can tailor your treatment, whether that's drug-free treatments (acupuncture, meditation, biofeedback, relaxation therapy), over-the-counter pain relievers, or prescription medications.
- What is a migraine?
Sometimes chronic pain has an obvious cause. You may have a long-lasting illness such as arthritis or cancer that can cause ongoing pain.
Injuries and diseases can also cause changes to your body that make you more sensitive to pain. These changes can remain even after you’ve healed from the original injury or disease.
Some people also have chronic pain that’s not tied to an injury or physical illness. Healthcare providers call this psychogenic pain or psychosomatic pain. It’s caused by psychological factors such as stress, anxiety and depression.
- What are the treatment options for chronic pain?
Treatment options for chronic pain may include over-the-counter drugs and topical treatments, prescription medications, injections, acupuncture, and prescribed exercises. Some people find relief for their chronic pain from alternative therapies, such as massage, meditation, and cognitive behavioral therapy.
- What types of medications may be used to treat chronic pain?
Your healthcare provider may recommend medications to relieve chronic pain symptoms, including:
- Anticonvulsants
- Antidepressants
- Corticosteroid
- Muscle relaxers
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen
- Topical products that contain pain relievers or ingredients that create soothing heat or cold
- Opioids
- Sedatives

Understanding chronic pain
Chronic pain can come in many forms. Learn more about common causes and treatment options.
- What is chronic pain?
Chronic pain is usually defined as any pain that lasts longer than three months This pain may occur all of the time or may come and go periodically. Chronic pain may affect people to the point that they cannot work, eat properly, take part in physical activity, or fully enjoy life.
- What is the difference between chronic pain and acute pain?
Acute pain happens when you get hurt, such as a cut or a broken bone. It doesn’t last long, and it goes away after your body heals from whatever caused the pain. Chronic pain, however, continues long after you recover from an injury or illness.
- What causes chronic pain?
One of the most important parts of treating headaches is figuring out your triggers. Learning what those are can help reduce the number of headaches you have. Try keeping a log of your headaches when they occur and note what you think caused them.
Once you know your triggers, your healthcare provider can tailor your treatment, whether that's drug-free treatments (acupuncture, meditation, biofeedback, relaxation therapy), over-the-counter pain relievers, or prescription medications.
- What is a migraine?
Sometimes chronic pain has an obvious cause. You may have a long-lasting illness such as arthritis or cancer that can cause ongoing pain.
Injuries and diseases can also cause changes to your body that make you more sensitive to pain. These changes can remain even after you’ve healed from the original injury or disease.
Some people also have chronic pain that’s not tied to an injury or physical illness. Healthcare providers call this psychogenic pain or psychosomatic pain. It’s caused by psychological factors such as stress, anxiety and depression.
- What are the treatment options for chronic pain?
Treatment options for chronic pain may include over-the-counter drugs and topical treatments, prescription medications, injections, acupuncture, and prescribed exercises. Some people find relief for their chronic pain from alternative therapies, such as massage, meditation, and cognitive behavioral therapy.
- What types of medications may be used to treat chronic pain?
Your healthcare provider may recommend medications to relieve chronic pain symptoms, including:
- Anticonvulsants
- Antidepressants
- Corticosteroid
- Muscle relaxers
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen
- Topical products that contain pain relievers or ingredients that create soothing heat or cold
- Opioids
- Sedatives
What medications may be used to treat chronic pain?

Anticonvulsants

Antidepressants

Corticosteroids

Muscle relaxers

NSAIDs or acetaminophen

Topical pain relievers

Opioids

Sedatives for anxiety or insomnia